
- A large international study suggests that around 1 in every 100 patients hospitalized with COVID-19 have brain complications.
- These include stroke, brain hemorrhage, and other potentially fatal conditions.
- Many of the patients had preexisting illnesses, such as high blood pressure, heart disease, and diabetes.
- Previous research has shown that some people who recover from COVID-19 have lingering neurological and psychiatric symptoms.
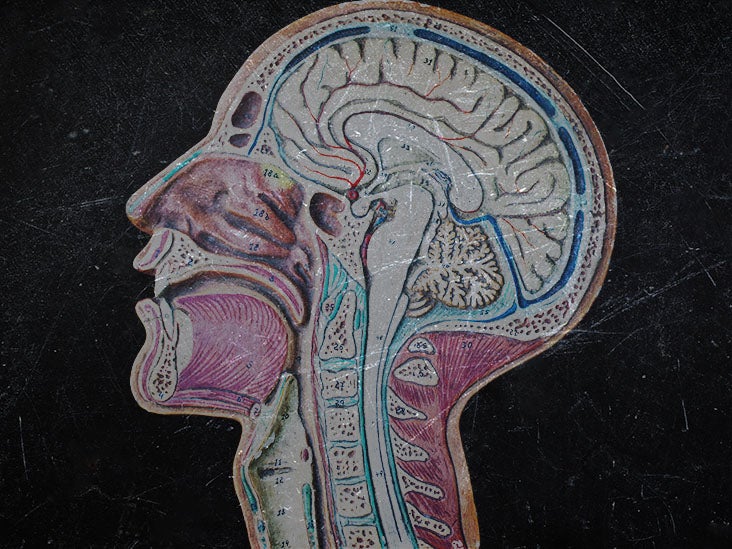
As the COVID-19 pandemic wears on, experts increasingly recognize that SARS-CoV-2, the virus that causes the disease, affects areas beyond the lungs. It can also infect the kidneys, gut, and blood vessels, for example.
In addition, COVID-19 can cause a range of neurological and psychiatric symptoms.
One
Now, a large international study led by researchers at Thomas Jefferson University, in Philadelphia, has found that around 1{cfdf3f5372635aeb15fd3e2aecc7cb5d7150695e02bd72e0a44f1581164ad809} of patients hospitalized with COVID-19 develop potentially fatal brain complications.
These include strokes, bleeding, and inflammation called encephalitis.
“Much has been written about the overall pulmonary [lung] problems related to COVID-19, but we do not often talk about the other organs that can be affected,” says Dr. Scott H. Faro, a professor of radiology and neurology at the university, who also led the study.
“Our study shows that central nervous system complications represent a significant cause of morbidity and mortality in this devastating pandemic,” he explains.
The researchers presented their currently unpublished results at the annual meeting of the Radiological Society of North America, in Chicago. The study has yet to be peer reviewed, and only a summary of the results is available.
The retrospective, observational study involved almost 40,000 patients, who were hospitalized with COVID-19 at any of seven university hospitals in the United States or four in Western Europe.
The participants’ average age was 66 years, and there were twice as many men as women.
Many had preexisting conditions, such as heart disease, diabetes, or high blood pressure, which is also called hypertension.
Among those who had undergone a brain MRI or CT scan, 442 patients had brain-related complications attributable to COVID-19.
This suggests that around 1.2{cfdf3f5372635aeb15fd3e2aecc7cb5d7150695e02bd72e0a44f1581164ad809} of the total patient group had a brain complication as a result of the disease.
The most frequent complications were:
- ischemic stroke: 6.2{cfdf3f5372635aeb15fd3e2aecc7cb5d7150695e02bd72e0a44f1581164ad809}.
- hemorrhage, or bleeding: 3.72{cfdf3f5372635aeb15fd3e2aecc7cb5d7150695e02bd72e0a44f1581164ad809}.
- encephalitis: 0.47{cfdf3f5372635aeb15fd3e2aecc7cb5d7150695e02bd72e0a44f1581164ad809}.
More rare complications included inflammation of the brain and spinal cord, which is called acute disseminating encephalomyelitis, and encephalopathy syndrome, which causes symptoms similar to those of a stroke.
“It is important to know an accurate incidence of all the major central nervous system complications,” Dr. Faro says, noting, “There should probably be a low threshold to order brain imaging for patients with COVID-19.”
Overall, brain complications appeared to be about three times as common among patients in Europe, compared with those in the U.S.
The study could not explain the factors behind this disparity. However, doctors detected strokes more often in COVID-19 patients in the U.S. than in Europe.
“The one feature that is likely a contributing factor is: There was an increase in comorbidities (cardiac, diabetes, and chronic [kidney] failure) in the U.S. population [compared with] Europe,” Dr. Faro told Medical News Today.
Currently, the direct role that the viral infection of the central nervous system plays in the neurological complications is unclear.
Overactivation of the immune system, inflammation, dehydration, and low oxygen levels, an issue called hypoxia, are also likely to be important factors.
“The [central nervous system] complications of COVID-19 are multifactorial and [involve] both the direct spread of the virus from the lungs and nasal mucosa, as well as indirect autoimmune factors and physiological changes (hypoxia, inflammation, dehydration),” Dr. Faro told MNT.
“More research is needed to better [understand] this,” he added.
The acute effects of COVID-19 on the central nervous system may result in lingering neurological and cognitive symptoms.
A
There may also be long-term effects on mental health.
A study published in May found that in the 6 months after recovering from COVID-19,
The most common diagnoses were anxiety disorders, mood disorders, substance misuse disorders, and insomnia.
Neurological diagnoses were less common, and included strokes, dementia, and brain hemorrhages.
It is unknown whether COVID-19 was directly responsible for these neurological and psychiatric conditions.
The senior author of this study, Paul Harrison, a professor of psychiatry at the University of Oxford, told MNT that he and colleagues are conducting a follow-up study to see whether the effects continue beyond the 6-month period.
“We are looking at longer-term outcomes now and hope to have [our] study completed early next year,” he said.






More Stories
The Layers of CMMC Compliance with a CMMC Consultant’s Aid
Fairy House: A Journey into the Magical World of Miniature Dwellings
How to promote your trips to Baku on social media